The enemy of our enemy: how oncolytic herpes could help cure cancer
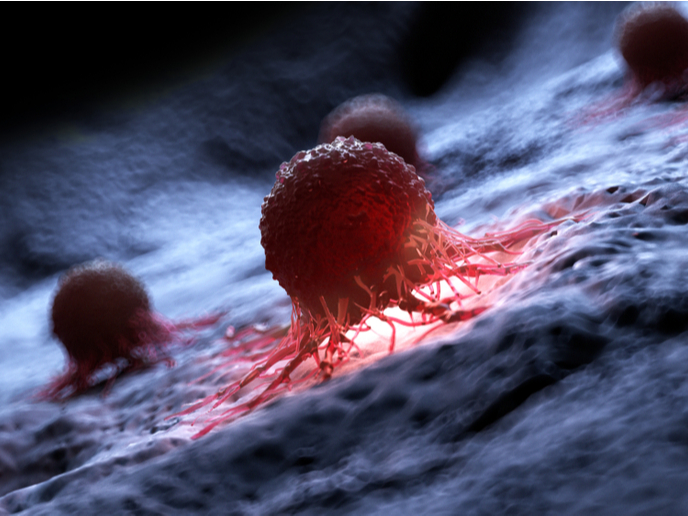
COVID-19 has shown us through bitter experience how resourceful a virus can be. But it’s just one of many examples. Did you know that some viruses can replicate selectively in cancer cells? These so-called oncolytic viruses (OVs) either evolved or were engineered in labs to make the most of cancer cells, as the latter oppose fewer obstacles to viral infections than healthy ones. Add this to a context in which the differentiation of cancer cells from normal ones has become the Holy Grail of cancer research, and you’ll start seeing the bigger picture. “In the OV field, the name of the game is to attenuate viral replication,” says Maria Gabriella Campadelli from the University of Bologna, European Research Council (ERC) grantee and principal investigator of the ONCOLYTIC-HERPES (Oncolytic herpes viruses retargeted to cancer-specific receptors) project. “The weakened OV replicates in and kills cancer cells and, to a large extent, spares non-cancer cells in the process.” Researchers have been trying to develop attenuated viruses to kill cancer for over two decades. One of them – currently the only one approved as a therapeutic drug – is a weakened herpes simplex virus (HSV) going by the name of T-VEC or ONCOVEX-GMCSF. Its safety, affinity for cancer cells and ability to treat patients multiple times without being blocked by their immune systems make it one of the most promising alternatives to treatments like chemotherapy and radiotherapy in melanoma patients. There is one problem. Forcing the virus to discriminate between normal and cancer cells has so far resulted in its weakening, thereby making it harder for it to kill cancer cells. Furthermore, it is effective only in a limited range of tumours. This is precisely why Campadelli’s team, prior to the ONCOLYTIC-HERPES project, had set out to genetically engineer HSVs that only infect and kill cancer cells. The prototype targets HER2 – a receptor in breast, ovary and other tumours – and destroys it.
Specificity vs attenuation
“Instead of attenuating virulence, we wanted to gain cancer specificity by modifying the virus tropism (how it responds to stimulus). Our ‘retargeted’ oncolytic herpes simplex viruses (oHSVs) enter cancer cells through molecules specific to their surfaces. They become ‘fully virulent’ in their target cancer cells and gain such selectivity by high cancer specificity rather than attenuation,” Campadelli explains. In this project, Campadelli intended to make oHSVs even better and eligible for a clinical trial. The first focus of her team consisted in devising a system for the production of retargeted oHSVs in non-cancer cells. “The HER2-retargeted oHSVs employed in preclinical studies were produced in cancer cells, and we knew that such a method would hardly be approved for a clinical-grade virus. We had to design novel retargeting strategies, and we opted for two sets of genetic modifications in the HSV glycoproteins which mediate virus entry into the cell. One modification enables the infection of producer cells through an artificial receptor we engineered, and the second modification enables the infection of cancer cells through the cancer receptor of choice,” points out Campadelli. In further efforts, the ERC-funded team demonstrated how oHSVs are extremely good at stimulating the antitumor immune response and making it much more responsive to checkpoint inhibitors (or combination therapy). Even though such a possibility remains to be tested, retargeted oHSVs could potentially be combined with Chimeric Antigen Receptor T-cells (CAR-Ts) for solid tumours. The team also showed how oHSVs could become a platform for other cancer receptors and ultimately target tumours of the breast, ovary, stomach, lung and pancreas, colorectal cancer, head and neck carcinomas, etc. Finally, the virus was found to be so cancer-specific that it is effective even upon general administration, at least in mice. With the project now completed, Campadelli hopes to find a company willing to invest in a first in-human clinical trial, likely in combination with checkpoint inhibitors. If successful, this clinical trial could mark a true turning point for curing cancer patients.
Keywords
ONCOLYTIC-HERPES, HSV, oncolytic virus, cancer, HER2, viral replication, retargeted, COVID-19