Transplanted nano-coated cells are a smart way to treat diabetes
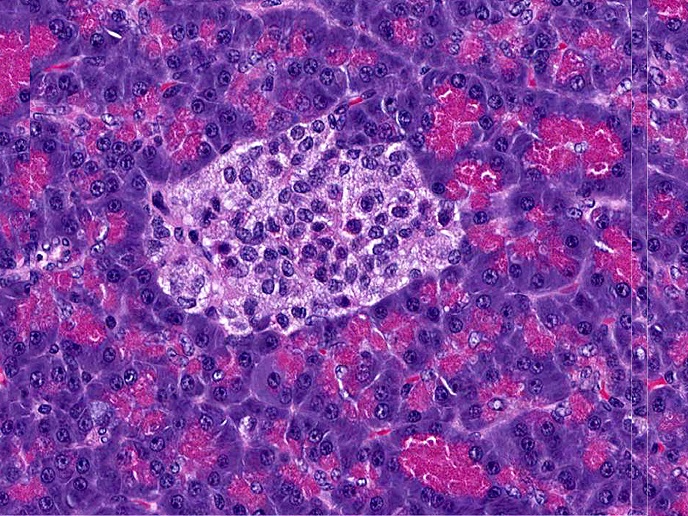
The pancreas plays an essential role in human health by producing and releasing insulin into the bloodstream to regulate blood sugar levels. However, in diabetic patients, the insulin-producing cells, present in specific pancreas structures known as ‘islets’, do not work properly. “A potential treatment for people with diabetes is to transplant islets from a deceased donor or other sources such as stem cells. But the problem is the transplanted islets are detected by the immune system which attacks them, and the implanted islets rapidly die,” explains José Carlos Rodríguez-Cabello, professor of condensed matter physics at the University of Valladolid, Spain and project coordinator of ELASTISLET (Tailored Elastin-like Recombinamers as Advanced Systems for Cell Therapies in Diabetes Mellitus: a Synthetic Biology Approach towards a Bioeffective and Immunoisolated Biosimilar Islet/Cell Niche). Treating islet-transplanted patients with immunosuppressants has not been very effective. Moreover, patients who have had diabetes since childhood would need to take immunosuppressants for life. Now EU-funded scientists have developed special bioengineered cells which are nano-coated with novel biomaterials. These protect the cells from the immune system, yet still allow them to deliver insulin to the blood stream.
Coating technology
The nano-coating does not completely isolate the islets. “It has to be selective, and permeable enough for oxygen, blood and nutrients to enter the cells and for insulin hormones produced by the islet to be released,” Rodríguez-Cabello points out. “We explored the applicability of a novel class of materials – elastin-like recombinamers – that are halfway between natural proteins and plastics,” Rodríguez-Cabello adds. Designed and produced synthetically, they have a protein-like nature that the islet can interact with at the cellular level when they are in natural surroundings, such as the pancreatic environment. Layer-by-layer technology creates a very thin coating by immersing the islets in a bath of a solution that has one of the components of the mixture. “Then you take it out and clean it a little so only a few molecules of this material remain on the surface and go to the second component which is complementary and which reacts with the first one,” explains Rodríguez-Cabello. With these washing and immersion steps, a very thin layer is created. “But we had to play a bit with the diffusion properties of the layer to achieve permselectivity,” Rodríguez-Cabello says.
Effective coating
Coating the cells was a challenge because of the irregular surface of the islet. “If you leave a hole big enough for the immune cell to detect, then all is lost,” Rodríguez-Cabello explains. So the team designed a system to improve coating efficiency. “We never arrived at 100 % coating efficiency, but we know that 80 % of the islets that we implant are well-coated and will stay for a long time.” The transplanted islets must also be able to interact with the surrounding cells and integrate with the host tissue. Integration is enhanced by a strategy to vascularise the cells allowing the development of blood vessels, which improves islets’ survival and the exchange of nutrients. Ninety-five researchers worked on the multidisciplinary project, 42 of them PhD students, including specialists in nanotechnology, immunology, cell biology, synthetic biology and bioengineering, as well as medical practitioners with clinical knowledge. By the end of the project, the team produced a system that works well in short-term experiments in laboratory animals and is now patented. “Now we are testing to see if these implants can retain this ability for longer periods, with the idea that you take this injection and it would last for a period of years. It could even eliminate the need for another injection,” concludes Rodríguez-Cabello.
Keywords
ELASTISLET, cells, immune system, immunosuppressants, diabetes, insulin, pancreas, Islet cells, biomaterials