New methodologies examine communication between brain regions in epilepsy patients to improve treatment
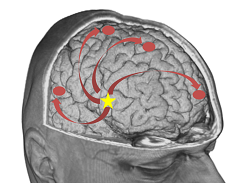
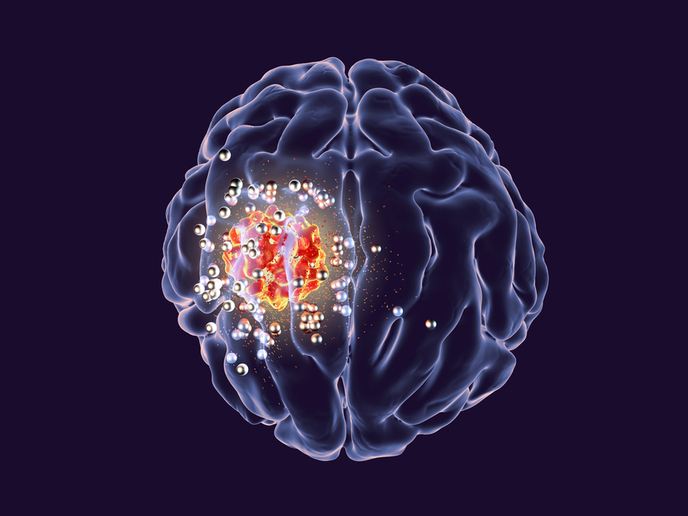
Approximately 30-40 % of patients with epilepsy can’t be adequately treated with anti-epileptic drugs. For these patients, surgery is the treatment with the highest effectiveness towards becoming seizure-free. The ability to accurately, quickly and efficiently estimate the epileptic focus is therefore of great importance. The EU-funded EPICONNECT project aimed at enabling the localisation of the region that generates the epilepsy by studying the functional interactions between the regions with electroencephalography (EEG). “This is important for achieving better treatment of epilepsy patients,” says project coordinator Stefaan Vandenberghe and Marie Skłodowska-Curie fellow Pieter Van Mierlo. “The patients can be treated more efficiently and earlier, allowing faster reintegration into public life and therefore reducing costs for society.” In clinical practice nowadays, the EEG is visually analysed by the treating neurologist. Localising the seizure onset zone (SOZ) from these EEG recordings isn’t currently possible in medicine. This is mainly because the EEG signals are polluted by muscle and movement artefacts during a seizure. Another reason is that the seizure rapidly spreads to other regions of the brain. In turn, this makes the visual localisation of the SOZ from EEG recordings an impossible task. Three-stage approach To address the problem, Ghent University and the University of Geneva implemented advanced EEG analysis techniques in the pre-surgical evaluation to localise the epileptic zone. In the first stage, they used a non-invasive tool called high-density electroencephalography to localise the seizure onset zone – the brain region that causes the seizures. In the second stage, the two partners adjusted the algorithms to standard low-density EEG that is recorded in all epilepsy centres worldwide. In the final stage they examined the influence of automated EEG analysis on the treatment management of patients. The researchers demonstrated that based on a 15-minute resting state EEG, the brain communication pattern obtained by EEG analysis allows to predict whether the patient has epilepsy or not with 90 % accuracy. Visual analysis couldn’t distinguish epilepsy from non-epilepsy patients. Furthermore, in the epilepsy patients, the side where the epilepsy originates from can be determined with 90 % accuracy. “In the long run, the improved diagnosis could mean that anti-epileptic drugs are started sooner in some patients when the epilepsy hasn’t manifested itself completely,” explains Dr Van Mierlo. “The sooner patients are treated, the better chance they have to become seizure-free and contribute to society.” At the same time, they demonstrated that the functional connectome technique yields greater accuracy in the localisation of the epileptic focus when compared with the standard EEG-based localisation technique. “EPICONNECT has the potential to impact the work of the epileptologist during the pre-surgical evaluation,” Dr Vandenberghe concludes. Algorithms designed and validated during the project can replace the visual analysis of EEG done by the epileptologist. “If these methods find their way to clinical practice, an extra tool will be at hand for the epileptologist to localise the SOZ or diagnose the type of epilepsy.”
Keywords
EPICONNECT, epilepsy, seizure, brain, electroencephalography, seizure onset zone, epileptologist