Cell sources for bio-engineered meniscus-like tissue
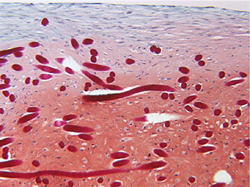
Injuries leading to disruption of the integrity of the protective meniscus in the knee joint can cause knee pain and ultimately osteoarthiritis. As the meniscus cushions and spreads the load in the knee, this can lead to disruption of the stability of the joint and significant loss in life quality. The overall aim of the European project MENISCUS REGENERATION was to emulate as closely as possible the structure of this vital tissue and engineer a tissue replacement. In order to achieve this, autologous cells would be bio-engineered on a bioactive and biodegradeable scaffold. Members of the consortium based at the Tissue Engineering Group in Basel, Switzerland performed trials on different cell types to deduce which would produce the most suitable replacement tissue graft. The cells selected for comparison were from human inner meniscus, fat pad, and synovial membrane. Articular chondrocytes were also used in the trials. The cells were induced to form tissue using a growth factor on a hyaluronan-based scaffold in vitro and using mice models. The resulting tissues were judged according to their glycosaminoglycan (GAG) content and correct production of collagen types in the different regions of the meniscus. As a reference, the collections of cells were compared with native human menisci. Only articular chondrocytes formed tissues with the necessary amounts of GAG and cell types compatible with both inner and outer meniscus cell phenotypes. Further research is required to fully test whether the tissue generated will attain the complexity of natural meniscus cartilage. However, other groups have applied the bio-engineered tissue in damaged sheep knee cartilage and extension of the trials with human meniscus repair was planned. The meniscus is a complex structure and advancements in tissue engineered for an effective biological implant would be welcome in the sports field and the ageing population generally. Figure caption: Cell Source: Representative Safranin-O stained sections of tissue generated by culture of articular chondrocytes into Hyaff®-11 for six weeks.