A more cost-effective way of treating osteoarthritis
Osteoarthritis is a chronic degenerative joint disease that affects an estimated 595 million people globally – with numbers continuing to grow. It is also the world’s fourth leading cause of disability. Currently, the gold standard for treating osteoarthritis is stem cell therapies. However, because these advanced therapeutics are expensive to develop and produce, their use in treating the disease remains limited. “Today’s manual production methods not only incur significant costs, particularly in terms of staffing, they also increase the risk of contamination due to the need for human intervention,” says Mary Murphy, a professor at the University of Galway. Clearly, what is needed is a better approach for both testing and producing advanced therapeutic medicinal products (ATMPs) – which is exactly what the EU-funded AutoCRAT project aimed to deliver. “We focused our work on closed automated systems, which cover the entire ATMP value chain, from the receipt of raw materials to the cryopreservation of the final product,” adds Murphy, who served as the project coordinator. “As such, we believe these systems have the potential to significantly reduce the risk of contamination while also lowering manufacturing costs – ultimately benefiting the patient.”
New regenerative therapies for osteoarthritis and cartilage repair
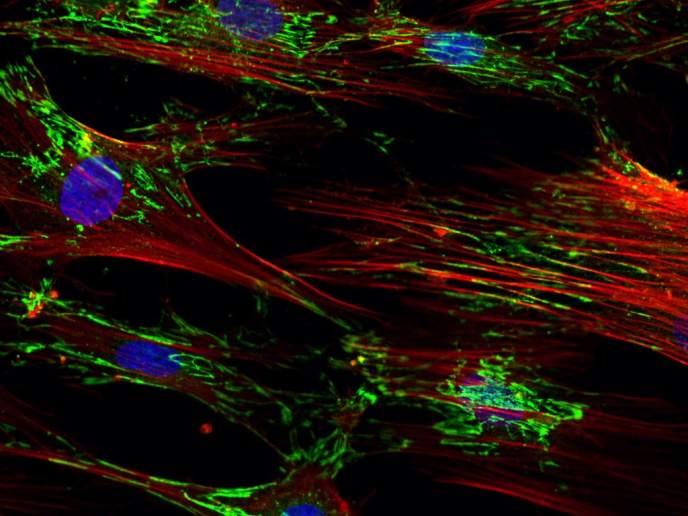
Using induced pluripotent stem cells (iPSCs), the project set out to develop new regenerative therapies for osteoarthritis and cartilage repair. “These cells have the ability to differentiate into any cell type in the body, making them an important tool in regenerative medicine,” explains Murphy. In the AutoCRAT project, human iPSCs were differentiated towards mesenchymal stromal cells (iMSCs), a type of stem cell that can differentiate into bone, cartilage, muscle and fat cells ex vivo, while also secreting reparative factors in vivo. In addition, researchers developed the capacity to isolate chondrocytes (iCHOs), the functional cells in cartilage. “While the iMSCs were used to treat established osteoarthritis, the iCHOs were used to repair injury-derived cartilage defects that could eventually develop into osteoarthritis,” remarks Murphy. Both MSCs and CHOs have been used to treat osteoarthritis in the past, but here they were used to prevent the disease from developing.
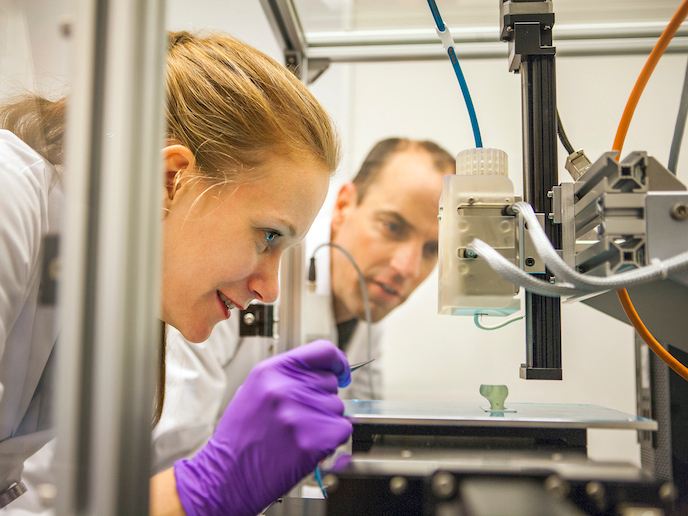
Automatically producing products for treating osteoarthritis
Another key outcome of the project was a closed, scalable and regulatory-compliant automated system. Called the AutoCRAT Regenerative Medicine Factory (ARM-F), this innovative solution is designed to enable the cost-effective production of the project’s groundbreaking therapeutic products. The automated production system covers cell production, the production of extracellular vesicles derived from the AutoCRAT cells, and the implementation of the quality control assays that ensure the functionality of any produced solution. “While the project’s ultimate outcome is the preclinical assessment of our therapies – an important first step towards human clinical trials – the ARM-F is what will ultimately allow us to produce these therapeutics in a closed and more economical way, making it more feasible to treat more osteoarthritis and other patients,” concludes Murphy. The project has produced numerous peer-reviewed publications and is in the process of drafting more.
Keywords
AutoCRAT, osteoarthritis, joint disease, stem cell, regenerative therapies, cartilage repair, advanced therapeutic medicinal products