A shining light for eye melanoma
Some chemotherapeutic drugs comprise metal centres such as platinum, which bind to DNA and inhibit replication and transcription. Alternative chemotherapy candidates have been proposed based on ruthenium. However, many metal-based compounds exhibit general toxicity due to the spontaneous activation before the drug reaches the tumour.
Ruthenium-based photoactivated chemotherapy
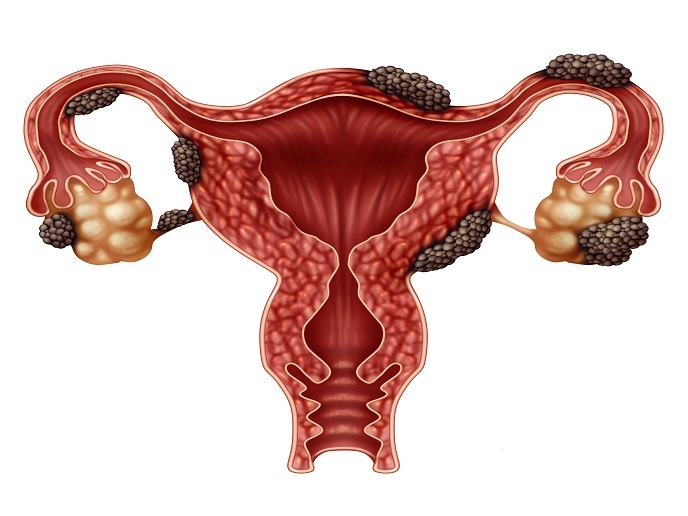
To ensure specific action of the drug on the tumour, scientists have conjugated these ruthenium drugs to organic molecules through a bond that is cleaved only upon light irradiation. When the bioactive, cytotoxic agent is coupled to a light removable protecting group, it becomes inactive as long as it remains in the dark. Using clinical techniques to irradiate tumours with light, the resulting ruthenium based photoactivated chemotherapy (PACT) agents show improved selectivity to the tumour by allowing activation of the chemotherapy drugs only, within the irradiated tumour cells, while the (non-irradiated) normal cells and tissues remain unaffected. Funded by the European Research Council (ERC), the Ru4EYE project capitalises on the light-activatable prodrugs developed during the RUPROLIGHT project. “Our goal during this project was to test whether these prodrugs could be used to treat eye cancer and, in particular, its most common form, uveal melanoma,” explains project coordinator Sylvestre Bonnet. Uveal melanoma is a rare malignancy of the eye with frequent metastasis to the liver. Despite treatment, survival is low (50 %) due to the metastatic form of the disease.
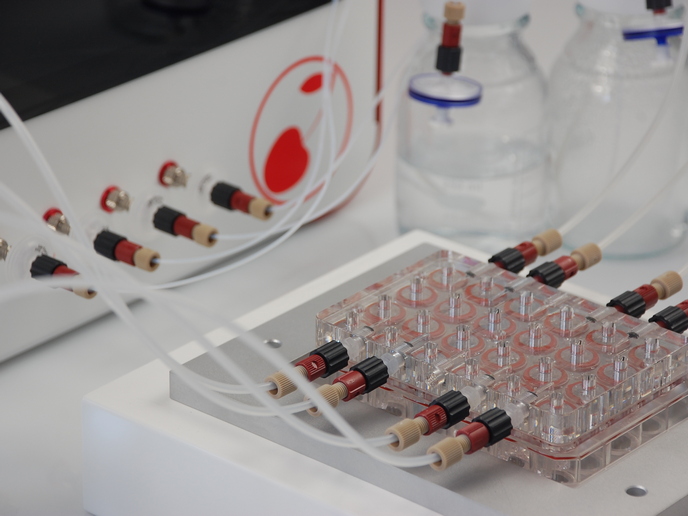
Compound screening in eye cancer models
The Ru4EYE experimental strategy initially involved the in vitro screening of numerous compounds using cancer cell cultures and 3D tumour spheroids. Following ruthenium prodrug administration and visible light irradiation, researchers observed the release of a photoproduct capable of triggering apoptotic cell death within 48 hours. The most efficacious candidates were selected for further in vivo testing in preclinical models. The team tested the PACT strategy in a zebrafish embryo-based model for conjunctival melanoma, another form of eye cancer. This work highlighted the importance of drug screening in vivo compared to in vitro. Furthermore, researchers developed a mouse model of eye cancer by inoculating human cancer cells under the skin of the animals. One of the tested compounds exhibited excellent anticancer activity not only against the primary eye tumour but also on liver metastases. Biodistribution experiments in mice demonstrated the fast excretion of the ruthenium prodrugs in less than 2 hours, while after 24 hours there were no detectable traces of ruthenium in the blood. Such fast clearance from the blood may also explain the absence of liver and kidney toxicity biomarkers, which altogether showed the low toxicity of this molecule towards mammals. “Our results confirmed that the caging strategy central to PACT is working: the ruthenium group attached to the chemotherapy molecule render the latter non-toxic,” emphasises Bonnet.
Taking photoactivated chemotherapy to the clinic
Translating new therapies into the clinic is the ultimate goal of nearly all research programmes of this type. Bonnet highlights the usefulness of such ERC proof-of-concept grants that make researchers think outside the box and consider business models and investments, next to scientific questions. The next step for Ru4EYE is to secure investments for the PACT technology. In collaboration with the RECORNEA start-up company, they plan to further develop the technology for clinical application. European funding, if granted, may become central to designing a treatment protocol, realising its full preclinical demonstration, and starting the corresponding clinical study, to bring the ruthenium-based PACT strategy for the treatment of uveal melanoma to the clinics.
Keywords
Ru4EYE, ruthenium, chemotherapy, PACT, uveal melanoma, prodrug, photoactivated chemotherapy, eye cancer, toxicity