EU-funded project to develop tiny particles that can deliver drugs directly to disease sites
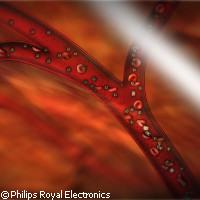
The EU-funded SonoDrugs project is developing tiny, image-guided capsules that will convey drug doses through the bloodstream to the site of disease, where they will be activated by ultrasound pulses. The new technology, which focuses on cardiovascular disease (CVD) and cancer, is expected to vastly improve therapeutic efficiency. The project has been financed with EUR 10.9 million under the Seventh Framework Programme (FP7) and brings together 15 academic and industrial partners from all over Europe. Cancer and cardiovascular disease are two of the most common causes of death; the EU recorded 1.9 million deaths from CVD in 2003 and 1.2 million from cancer in 2004. Current treatments rely on 'whole-body' doses that are difficult to control and often come with undesirable side effects. One of the goals of SonoDrugs is to ensure that drugs targeting cancer or cardiovascular disease provide the maximum benefit to the patient by being activated only where they encounter diseased tissue. This should certainly improve the efficiency of delivery, but it also avoids the problem of dosing all of the body's major organs. The researchers are working to develop microscopic (100-2,000-nanometre-diameter) drug-loaded capsules that can be delivered through the bloodstream to diseased tissue, where they can release a dose of the drug on command. The very small size of the capsules allows them to be conveyed through the smallest blood vessels and well into the diseased tissues. The drug doses will be contained either within the particles themselves, or somehow attached to the shell. Two particles will be designed: one with a shell that melts in response to the local heating effect of ultrasound, and a larger one that ruptures under pressure from ultrasound pulses. A different version of this second type of particle, often referred to as a 'microbubble', is already in use as a 'contrast agent' in ultrasound imaging. Real-time magnetic resonance imaging (MRI) will be used to detect the arrival of the capsules at the desired destination. MRI is ideally suited to the project because it measures local tissue temperatures, locates lesions and tracks labelled particles easily. Once at their destination, the drug-loaded particles will be forced to release their dose, either by the heat or pressure from focused ultrasound pulses. SonoDrug's MRI-guided drug delivery efforts focus on treatments for cancer; MRI techniques will be developed that will simultaneously detect the arrival of the labelled, drug-loaded particles at the disease site; measure the heating effect of ultrasound pulses; and monitor the temperature-triggered release of drugs from the particles. The partners will explore potential treatments for CVD using ultrasound as both the primary imaging modality and the trigger for drug release from the pressure-sensitive microbubbles. One of the project partners, Philips Royal Electronics, will adapt its existing microbubble technology to deliver drugs; SonoDrugs will also make use of its integrated MRI/ultrasound research system. 'New therapeutic options such as externally triggered local drug release at the specific site of disease hold the promise to significantly improve patient care,' said Henk van Houten, senior vice president of Philips Research. 'We realise that medical imaging technologies are only one of the 'enablers' required to fulfil this promise. However, the wide-ranging expertise that has been brought together in the SonoDrugs project puts us in a strong position to ultimately deliver the benefits of image-guided drug delivery to patients and care providers.' The researchers will also examine the potential of gas-filled microbubbles to increase the uptake of drug doses at the target sites in a process called 'sonoporation'. Sonoporation occurs when gas-filled microbubbles fracture in response to the stress induced by an ultrasound pulse; when this happens near a living cell, the cell's wall is impacted and becomes more porous. This makes the cell more willing to let in large drug molecules. This process is potentially quite useful for reducing the necessary doses in conventional 'whole-body' drug delivery. The way it works is not yet completely understood, and forms an exciting area of investigation for the project.