The role of our gut biome in our health and well-being keeps unfolding
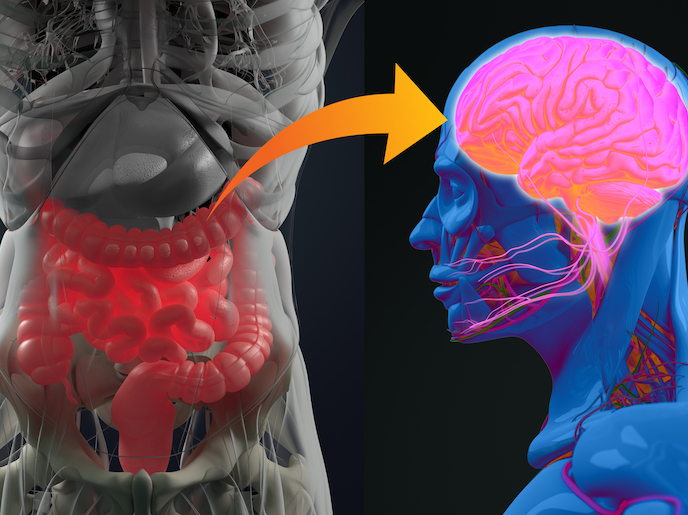
The MyNewGut project received support from the EU to shed light on the contribution of the human microbiome to nutrient metabolism and energy balance. Project coordinator Prof. Yolanda Sanz, head of the Microbial Ecology, Nutrition & Health Research Unit based at the National Research Council (IATA-CSIC) in Valencia, explains: “We also wanted to identify microbiome-related features that contribute to, or predict, obesity and associated disorders. We looked at how the microbiome is influenced by environmental factors and its role in brain and immune development and function in humans.” One case study conducted by the consortium involved the transference of gut microbiota from healthy donors to subjects with metabolic syndrome via faecal microbiota transplants (FMT). They demonstrated that a ‘healthy microbiota’ increases the striatal dopamine receptor expression in the brain (SPECTscans), which is a system involved in improved appetite control. This led to reductions in food intake in a human intervention trial. “The findings demonstrate one of the causal mechanisms whereby the gut microbiota positively impacts energy balance and so improves metabolic health,” explains Prof. Sanz. “These findings could enable researchers to specifically target the gut-brain axis. This could be done either by diets that enrich our gut microbiota with these bacteria, or by providing the identified bacteria or metabolites as novel therapeutics. This could beneficially change food intake and behaviour in humans in the future.” High-protein diets (HPDs) are all the rage at the moment. The project considered their impact through a randomised double-blind, placebo-controlled, parallel-design intervention trial. This investigated the effects of both the amount and types of proteins (casein or soy protein) on healthy, overweight volunteers. “Although HPD are often effective for losing body weight, the increased protein intake also increases the proportion of protein products that reach the large intestine and are metabolised by the colonic microbiota. This generates toxic compounds, which also depend on the protein type, and should be considered in dietary recommendations.” Their findings are extensive, and highly relevant to our modern lifestyles. Through a longitudinal study conducted in children, the consortium also considered the impact of an unhealthy diet, including a high intake of simple sugar and fat. This is associated with a low-diverse microbiota and heightened inflammation in normal weight children who later develop obesity, compared to children who remained normal weight. “This finding suggests that the gut microbiome is part of the individual’s features that contribute to predicting normal or excessive body weight gain and obesity onset. This information could help in early detection of obesity risk and the implementation of early dietary preventive measures.” MyNewGut consortium members demonstrated that young adults born by C-section have higher stress responses than those who were delivered vaginally. “This is of importance given the relationship between stress and mental and metabolic illness and the C-section rates, which are increasing globally.” C-section rates in the EU exceed 30 % while levels of around 12 % are recommended by the World Health Organization. They showed a clear negative impact on the neurodevelopment of young children combined with antibiotic use in the first few days of life. The project’s identification of new bacterial strains could give rise to a new generation of probiotics, able to tackle obesity and its metabolic complications more effectively. “The biobank of human indigenous gut bacteria generated by the CSIC harbours valuable biological material, which can be exploited further for future applications in nutrition and clinical practice.”
Keywords
MyNewGut, probiotics, gut bacteria, microbiota, high-protein diets, gut microbiome, gut-brain axis