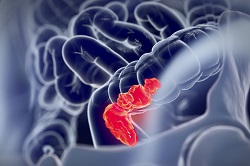
New, tumour-specific therapy for colorectal cancer patients
Preventing relapses for colorectal cancer – the second most deadly form of cancer in Europe – is complex to say the least. The reasons for such relapses can vary: spreading of isolated cancer cells beyond the primary tumour site; remaining cancer cells at this site following its resection; poor specificity of post-resection chemotherapy; or resistance to chemotherapeutic treatments. Yet, Dr Helena Azevedo of Queen Mary, University of London (QMUL) believes that, whatever the cause, such relapses can be prevented with post-therapies promoting the regeneration of the damaged tissue. Enter CANCERHYDROGELPATCH, an EU-funded project whose purpose was to target colorectal tumours cells with hydrogels-drug-siRNA nanorods conjugates after surgical removal of the tumour. ‘Our idea was to design a therapy customised for a particular cancer, to be more effective and safer,’ says Dr Azevedo. ‘For example, it is known that growth factors – proteins involved in cell proliferation – are typically overexpressed in most tumours, contributing to cancer progression and spreading. Using Bevacizumab, also known as Avastin, we saw that we could prevent tumour growth. But the complexity of the tumour environment requires the delivery of multiple therapies, so we selected an additional drug consisting of short interfering RNA (siRNA – able to supress/knockdown the expression of specific genes) with the aim of silencing an important oncogene implicated in the progression of colorectal cancer.’ Although drugs like Avastin are already being used in patients with colorectal cancer, CANCERHYDROGELPATCH innovated by not administering it systemically or by intratumoral injection – a practice that results in adverse side effects through non-specific uptake by both healthy and cancer cells, and accumulation in other organs. Instead, the team aimed to deliver these drugs within a hydrogel at the desired site and selectively to cancer cells by attaching them to nanoparticles coated with small peptide molecules that bind specifically to the surface of cancer cells. ‘The results were outstanding,’ Dr Azevedo enthuses. So outstanding in fact, that the team exceeded its initial expectations of a therapy that could be applied after tumour resection. Their combinatory therapy boasts high efficacy in both resected and non-resected tumours by combining three therapeutic approaches: gene therapy to silence oncogenes involved in cancer progression; chemotherapy involving the release of a potent drug that stops growth of cancer cells; and thermal therapy that produces heat and kills cancer cells. ‘It was shown that this triple therapy was able to promote tumour abrogation, eliminating the need for their resection. When applied post-resection, complete remission was achieved by destroying the remaining cancer cells and avoiding tumour regrowth,’ says Dr Azevedo. The new therapy generated so much enthusiasm in the community that it led to the publication in the leading journal ‘Nature Materials’. Now, Joao Conde, who participated in CANCERHYDROGELPATCH and specialises in designing and testing nanobiomaterials for cancer treatment, is bringing together a new research group to further develop these therapies. ‘Whilst the results in mice are very promising in terms of efficacy and safety, further validation of the therapies in large pre-clinical models that allow for follow-up studies over longer periods is necessary before we can bring our new treatment and delivery method to human patients. This might require 5 to 10 years, if everything goes as expected,’ Dr Azevedo concludes.
Keywords
CANCERHYDROGELPATCH, colectomy, colorectal cancer, tumour, metastasis, chemotherapy, hydrogel, Avastin, siRNA, gene expression, peptide, resection