Small microbial players with a big impact on obesity
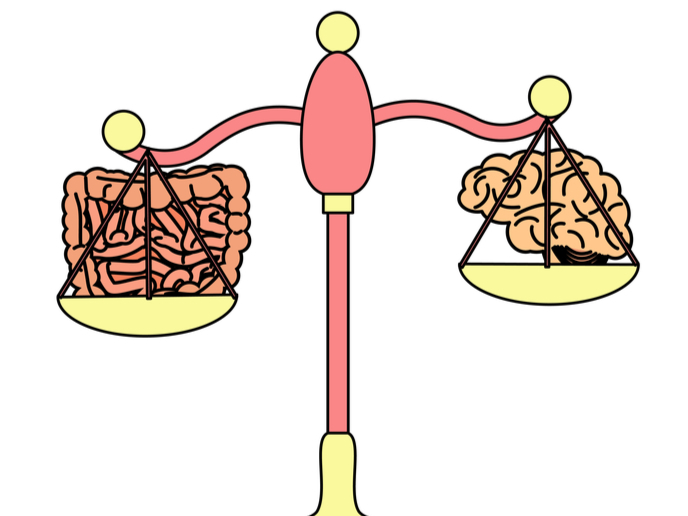
Despite the knowledge that microbiome-based strategies could be harnessed to tackle metabolic health and obesity, there is still an acute lack of understanding as to how gut microbiota interact with their host. The most interesting revelation recently is that the so called ‘gut microbiota–brain’ axis involves a network of connections that allows two-way communication between gut bacteria and the brain. Evidence suggests that vagal afferent nerve terminals in the gut wall sense nutrient-related hormonal and/or mechanical signals.
Bacterial players in the energy metabolism arena
Supported by the Marie Skłodowska-Curie Actions programme, the miVaO project investigated the role the gut microbiota plays in the regulation of nutrient sensory transmission from the vagal nerves of the gastrointestinal tract to the brain. The next step was to identify the key bacteria responsible for energy balance. “The ultimate goal is to contribute to developing more effective interventions to tackle obesity,” says Yolanda Sanz, professor at the Spanish National Research Council and project coordinator. miVaO researchers successfully identified a key microbial player, Holdemanella biformis. In a diet-induced obesity mouse model, this bacterium improved the functioning of the glucagon-like peptide 1 (GLP-1) system and induced anti-diabetic effects – improving glucose tolerance.
Sensory neurons with an impact on obesity
The researchers generated a mouse model without NaV1.8-expressing neurons. The intention was to show that H. biformis induces its glucoregulatory effects through vagal afferents. “However,” as Marina Romaní-Pérez, main researcher of the project explains, “the absence of NaV1.8-expressing neurons interfered with the normal development of diet-induced obesity in mice, so we could not use this model for its initial purpose.” Instead, they better characterised the impact of NaV1.8 ablation on the control of energy homeostasis through microbial, endocrine and immune signals. The absence of NaV1.8 neurons improved some metabolic parameters under a low-calorie diet, with gender-dependent effects. “While females showed improved oral glucose tolerance, males had partial resistance to gain weight,” Romaní-Pérez notes. Overall, for control of food intake, glucose tolerance, lipid storage and intestinal immune response, the team found that the sensory neurons expressing NaV1.8 channels are required. Moreover, two types of T cells, regulatory T cells (Treg) and T helper 17 cells (Th17), are involved in this delicate balance. Based on this evidence, the researchers hypothesise that gut microbiota, throughout their interactions with the diet, prompt diurnal or twice-daily oscillations of nutrient and immune-related signals rapidly transmitted to the brain through NaV1.8-expressing neurons. Importantly, this act as a brake on appetite and ultimately terminates food intake and modulates intestinal immune response according to the individual’s nutritional status.
Future research will highlight personalised microbe therapy
The team are continuing their work on this facet of food intake control. Faecal samples are still being analysed by 16S rRNA gene amplicon sequencing and metabolomics approaches to identify gender dependent microbial mechanisms behind the vagal afferent control of glucose homeostasis and lipid intestinal uptake and metabolism. Sanz is keen to pursue the avenues opened up by miVaO investigations. She concludes: “We would like to continue researching the dynamic relationship between gut microbiota and the host. Then, we could design personalised microbiome-based interventions to enhance gut-brain communication for better adjustment of energy homeostasis at mealtimes.”
Keywords
miVaO, obesity, gut microbiota, NaV1.8, vagal nerve