New study highlights immune system's role in Alzheimer's
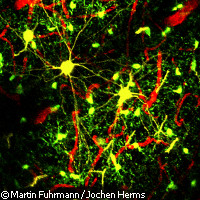
The brain's immune cells may be behind the loss of neurons associated with Alzheimer's disease, new EU-funded research suggests. The findings, published in the journal Nature Neuroscience, could lead to the development of new treatments for the neurodegenerative disease. EU support for the work came from the NEURO.GSK3 ('GSK-3 [glycogen synthase kinase 3] in neuronal plasticity and neurodegeneration: basic mechanisms and pre-clinical assessment') project, which has been allocated EUR 3.57 million under the Health Theme of the Seventh Framework Programme (FP7). Alzheimer's disease is a leading cause of dementia among the elderly; as many as 18 million people worldwide suffer from the condition, and this figure is set to rise as our populations age. The disease is characterised by the progressive, irreversible loss of nerve cells from the brain and the build-up of proteins in beta amyloid plaques and tangles. Known as microglia, the immune cells of the brain are able to destroy the beta amyloid plaques associated with Alzheimer's disease. However, the microglia are also known to kill off brain cells in mice with other neurodegenerative conditions such as Parkinson's disease. In this study, scientists from Ludwig-Maximilians-University (LMU) in Germany and the University of California at Irvine in the US set out to determine whether the microglia were more friend or foe in Alzheimer's disease. Their research subjects were mice with a rodent version of Alzheimer's disease. Crucially, the mice had been genetically modified so that their brain cells fluoresced yellow while their microglia glowed green. This allowed the scientists to easily follow the fate of the brain cells and microglia in the mice over a period of one month. Over the course of the experiment, it became clear that the microglia gather around the neurons before, and not after, the brain cells begin to die. The researchers suspected that as the disease progresses, stressed nerve cells send out a chemical messenger that attracts the microglia. These spark off an inflammatory reaction which brings about the neurons' demise. 'We assume that the sick nerve cells near plaques secrete a chemical messenger that induces the microglia to home in on them,' explained Professor Jochen Herms of the LMU's Center of Neuropathology and Prion Research. 'The best candidate for the messenger responsible is the chemokine fractalkine, which docks onto a receptor protein on the surface of the microglial cells.' To test this idea, the team repeated the experiment in mice lacking the Cx3cr1 gene which makes the receptor on the surface of the microglia. This time, nerve cell loss was prevented, demonstrating that communication between the nerve cells and microglia is an important factor in the development of Alzheimer's disease. Professor Herms concluded: 'We may be able to make use of these results to develop novel agents that can slow the rate of neuron loss by interrupting communications between the two cell types.' Symptoms of Alzheimer's disease include memory loss, confusion, language difficulties and changes in behaviour. As the disease progresses, these symptoms worsen until patients are largely bedridden and unable to take care of themselves. There is no cure for Alzheimer's at this time.
Countries
Germany, United States