Imaging technique offers cancer patient screening for nanomedicine therapies
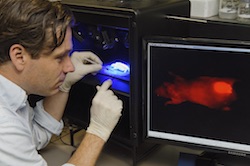
A significant barrier for the nanopharmaceutical industry tackling cancer is that while some patients treated with nanomedicine (NM) show major improvements in survival rates and quality of life, many others do not respond well. This can result in delays to those patients receiving appropriate treatment. An effective mitigation would be the ability to stratify likely responders from non-responders, prior to their selection for studies or treatment. The EU-funded CONQUEST (Companion Nanodiagnostics for Quantifying EPR and Stratifying Patients to Targeted Nanotherapies) project addresses this clinical gap through the development of nanomedicine imaging which uses (radio-)tracer labels to pre-select patients for inclusion in clinical trials. Additionally, market research amongst opinion leaders to ascertain which tracers, imaging methods, clinical protocols and reimbursement models were preferred has enabled the team to propose therapeutic solutions. Individual EPR profiles for each tumour Nanomedicines depend on the so-called Enhanced Permeability and Retention (EPR) effect to work, whereby molecules are thought to accumulate more readily in tumours than in normal tissue. However, the EPR effect is variable across patients and can even present differently within lesions in the same patient. Unlike virtually all new anticancer drugs which have protocols to stratify potential responders from non-responders, nanomedicine tumour-targeting technology does not have the same safeguard. CONQUEST was able to conduct non-invasive imaging of tracer-labelled nanocarriers that accumulate in tumours through the EPR effect. Patients evidencing a low degree of EPR, and so unlikely to respond, can then be excluded from treatment and referred for established or experimental interventions. Likewise, patients with a high level of EPR can expect relatively impactful treatment. “Pre-selecting patients in nanomedicine trials ensures that promising formulations transit more efficiently from phase one to two and three, and that only patients most likely to respond will be treated with the drug delivery system in question,” explains Professor Twan Lammers the project’s principal investigator. The team applied both nanodiagnostic and nanotheranostic approaches. In the former case, drugs are precluded from the nanocarrier screening step. Whereas with the theranostic approach, both the drug and the imaging agent are present in the same formulation, providing valuable in situ information on target site accumulation of the nano-drug under investigation. “Options are currently being explored, by us and others; not only in terms of making and upscaling the therapeutic application of nanoproducts, but also for defining the optimal biomarkers and measures to be used for patient pre-selection,” Prof. Lammers summarises. “These include things like the percentage of injected dose, distribution of dose within the tumour and the kinetics of probe accumulation.” A key therapeutic tool for the future To exploit the technology’s commercial potential for the pharmaceutical and diagnostics industry, the CONQUEST team is working to customise the technique for integration with PET-MRI imaging. However, as well as being the most promising, it is also the most difficult, costly and least available imaging technology and so they are also weighing up the pros and cons of using PET-CT or SPECT-CT. “In future, theranostic techniques are likely to be used to exploit nanomedicine more efficiently in the clinic, for immunotherapy purposes,” Prof. Lammers enthuses before adding, “We are currently exploring several options in this direction. Nanomedicine is still in its infancy, but with increasing discussion and success stories, I am convinced this will become a crucial therapeutic tool for cancer patients.”
Keywords
CONQUEST, Nanomedicine, cancer therapy, tumour, drugs, imaging, clinical trials, nanocarriers, nanodiagnostic, nanotheranostic, biomarkers