An effective combination therapy against dangerous sandfly-borne disease and HIV
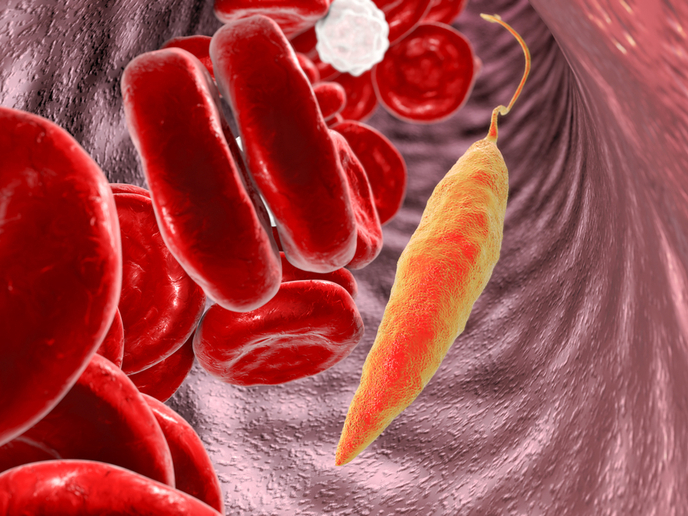
Visceral leishmaniasis (VL) is a parasitic disease that can kill if left untreated. Found mostly in Brazil, east Africa and south-east Asia, it’s second only to malaria in the number of deaths it causes. It’s difficult to treat to begin with, but VL becomes even more of a challenge in patients with HIV. The HIV virus increases the incidence of VL, makes it more severe and causes more relapses, increasing the likelihood of death. A team of researchers supported by the EU-funded project AfriCoLeish has been investigating appropriate treatment strategies for VL-HIV co-infections in Ethiopia, a country with the highest global incidence of VL in people living with HIV. A recent clinical trial on co-infected patients conducted by the team has demonstrated that their proposed combination therapy shows promise as a safe and effective treatment for sufferers. The results of the trial have been published in ‘PLOS Neglected Tropical Diseases’. A look at the disease Leishmaniasis is caused by parasites spread by the bite of infected female phlebotomine sandflies. VL, also known as kala-azar, is the most serious form of the disease, causing irregular bouts of fever, significant weight loss, anaemia, and swelling of the liver and spleen. According to the World Health Organization (WHO), there are about 50 000 to 90 000 new cases of VL worldwide each year. If left untreated, the death rate can be as high as 100 % in developing countries. A combination therapy The current WHO-recommended treatment for VL-HIV co-infection is 40 mg/kg of the injected drug liposomal amphotericin B (more commonly known as AmBisome). The project team, which was coordinated by the Drugs for Neglected Diseases initiative (DNDi), wanted to see if a lower dose of AmBisome combined with the orally administered miltefosine would have positive treatment results. In their randomised trial, they tested both the WHO-recommended treatment and the combined therapy of AmBisome (30 mg/kg) and miltefosine (100 mg/day for 28 days). Results showed that the combined treatment was much more effective than AmBisome taken on its own. A parasite clearance of 67 % was achieved when treatment lasted 28 days (compared with the monotherapy’s 50 % cure rate). This increased to 88 % (compared to a much lower 55 % for the monotherapy arm) when patients who had improved but still had the parasite received a second round of treatment (lasting another 30 days). “Considering the individual and public health benefits, there is a strong case for the prompt adoption of this treatment in international and national guidelines,” said DNDi Senior Leishmaniasis Advisor Dr Jorge Alvar in a press release posted on the DNDi website. “The results also suggest a new case management strategy is needed, whereby using one or two rounds of treatment depends on whether negative parasitology has been achieved.” Four European and two African partners contributed their vast research and medical expertise to AfriCoLeish (Care Package for Treatment and Control of Visceral Leishmaniasis in East Africa) during its 4-year term. The project ended in 2016, but its members are continuing their work on more efficacious treatments for VL-HIV sufferers. For more information, please see: AfriCoLeish project website
Countries
Switzerland