Imaging cell fate after cell therapy
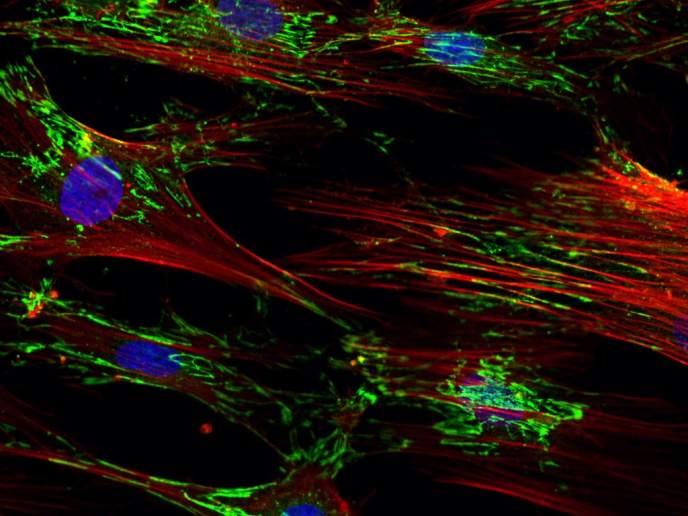
An escalating interest in cell therapy has been triggered by the realisation that transplanted cells could be used for regenerative purposes, as an active drug or as a drug delivery vehicle. Whatever the ultimate application, it is vital to be able to deliver these cells efficiently to the target organ and monitor their fate in order to understand the mechanisms of how cell therapy works. Magnetic resonance imaging (MRI), despite being a very powerful tool in clinical diagnosis and biological research, has limited sensitivity for tracking the fate of cells. To address this issue, the EU-funded 'European network for cell imaging and tracking expertise' (ENCITE) project aimed to improve on existing methods and develop new ones based on magnetic resonance (MR) and optical imaging for monitoring cell fate. Ultimately, the project goal was to be able to take these techniques to the clinical environment and apply them in the treatment of stroke and neurological, cardiovascular and musculoskeletal diseases as well as diabetes and cancer. Among the project's objectives was to increase the number of reporter genes available for MRI and to develop non-invasive imaging methods for the detection of processes such as cell migration, differentiation, proliferation and death. Partners were interested in generating new reagents, such as iron oxide nanoparticles, paramagnetic metal complexes and fluorine-containing compounds, that would improve the sensitivity and specificity of cell labelling. A new imaging reporter gadolinium (Gd)-based agent was shown to provide an impressive seven-fold sensitivity enhancement in comparison to commercially available agents. New techniques for cell labelling were also devised, including photochemical internalisation (PCI) with minimal interference with the cells' migratory and functional properties. Pioneering non-linear imaging modalities were formulated that enabled the detection of tissue structure and function by multi-photon microscopy. The light excited by collagen fibres and actomyosin bundles was combined with infrared light for the detection of tissue interfaces including adipocytes, nerve tracks, erythrocytes and collagen. This technology was successfully used to map the invasion routes of cancer cells during metastasis. Pre-clinical validation of the imaging methods entailed the generation of tools that would facilitate monitoring of the migration, integration, functional status and differentiation of the transplanted stem cells. Labelling of pancreatic islets by superparamagnetic iron oxide nanoparticles allowed the successful MR imaging of these cells in an animal model, demonstrating the potential of these techniques to be applied for patients with type 1 diabetes. Tools developed by ENCITE would be used for monitoring any improvement outcome following cell therapy, including organ function. Other applications include the monitoring of immune responses following cancer immunotherapy.