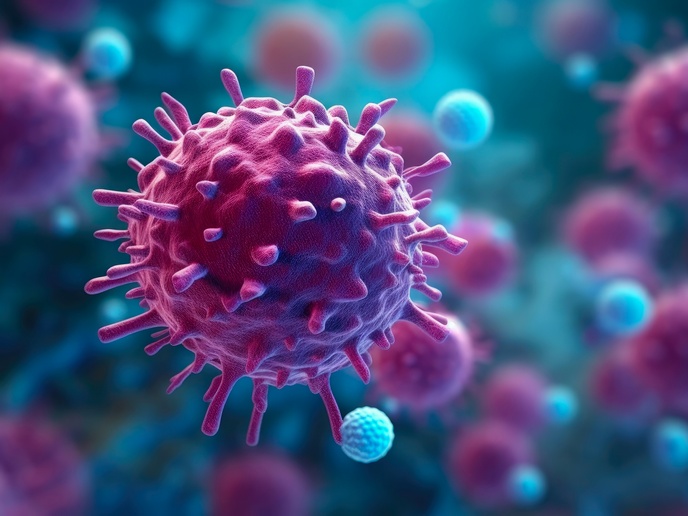
Wood dust inflammation in lungs
Exposure to any agent causing inflammation gives rise to a cascade of biochemical and cellular changes. This is characterised by a whole array of cells and proteins that rush to the site of exposure in response to the harmful stimulus. White cells include macrophages, lymphocytes, neutrophils and eosinophils. The protein line-up associated with inflammation includes cytokines and chemokines. Project partners at the Finnish Institute of Occupational Health looked for these indicators of inflammation in a mouse model in vivo and in vitro. Trials monitored responses to both hard and soft wood dust. In particular, they compared the responses to two types of wood commonly used in the furniture industry - birch and oak. In vitro studies involved observations of a mouse cell line for changes that indicated an immune response. In this case, they found that birch was a stronger inducer of the proteins cytokines and chemokines. Analysis of in vivo studies showed that both oak and birch induced the whole battery of cells associated with an inflammatory response. However, quantitative and qualitative measurements suggested that there was a differential response for different woods. This time, oak dust was implicated as a stronger promoter of proteins indicating inflammation. Overall the study indicated that repeated exposure to wood dust could influence the development of allergic asthma through the modulation of white blood cell proteins. The differential response to different types of soft and hard wood will no doubt be instrumental in setting limits for some 3.6 million workers involved in the wood products industry in Europe.