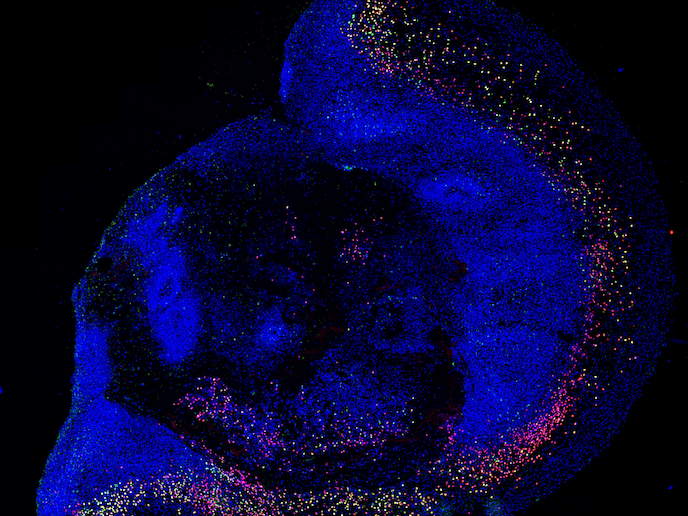
Brain organoids offer robust 3D models to study human neurodevelopment
A barrier to better understanding autism and other neurodevelopmental disorders is that researchers cannot access live human brain tissue to study these conditions at the molecular and cellular level. This has led to reliance on animal models that are not fully comparable with humans. However, the Marie Skłodowska-Curie Actions supported ProTeAN project was able to benefit from recent breakthroughs in the use of stem cells to create 3D models called organoids. Organoids are capable of mimicking human brain development. They are also able to acquire mature brain functions, such as the formation of activated neuronal networks. The team generated brain organoids from dental stem cells, taken from milk or wisdom teeth. “This model leads us to believe we are on the right track to a better understanding of the human biology of neurodevelopmental disorders,” says Catarina Seabra. She is the project fellow from the Center for Neuroscience and Cell Biology, at the University of Coimbra in Portugal, which hosted the project. The team established the first dental stem cell biobank in Portugal for the study of brain disorders. They received ethical approval from both the Pediatric Hospital of Coimbra and the University of Coimbra. The approval allowed for the reprogramming of cells to ensure their ability to become virtually any cell type, known as pluripotency. The biobank includes dental stem cells that were collected from both autistic patients and control groups. These had already proved a critical resource for the EU-funded Syn2Psy project. The team have been interviewed on national TV channels, such as RTP (website in Portuguese) and SIC (website in Portuguese). These programmes reached an audience of over a million people in Portugal.
From dental stem cells to brain organoids
ProTeAN’s goal was to develop brain organoids which would allow the neurons, the building blocks of the brain, to grow in a 3D environment and form the complex structures that occur in humans. The organoid’s composition, alongside neuronal properties such as complexity and communication, could then be tested in the lab. By comparing patient with control samples, this could reveal what is altered during neuronal development or communication in autism. To ensure their suitability, the dental stem cells were characterised by flow cytometry to identify proteins on the surface of the cells and by qRT-PCR, to detect the proteins coded by the genes. These cells were then induced to become pluripotent stem cells and then used to make the 3D brain organoids. “We established key timeframes to better understand the milestones of organoid development. We learned that at three months, brain organoids expressed mature neuronal markers. This indicates their potential as robust neurodevelopment models. But we only saw complex electric activity in six-month organoids,” adds Seabra.
Towards personalised medicine
Work done by the project could contribute to the improved health and well-being of all those living with these neurodevelopmental disorders, reducing their social and economic impact. “In the future we expect to use patient-derived brain organoids to design and test personalised therapies. Right now the focus is to improve our understanding of molecular and cellular changes in neurodevelopmental disorders at a fundamental level,” explains João Peça, the project’s supervisor. Towards this end, the team are analysing patient cells from their biobank with genetic alterations associated with autism risk, to further understand the neuronal circuitry and biological pathways affected by these genetic changes.
Keywords
ProTeAN, organoid, autism, neurodevelopmental, neuron, brain, 3D model, stem cells, pluripotent, personalised therapies, biobank