Alzheimer's-linked protein can travel into brain, study shows
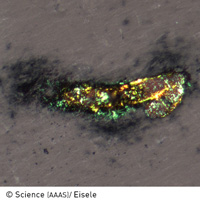
Researchers have discovered that tissue from outside the brain that contains misfolded beta-amyloid protein can travel and 'infect' the brain. Pathological protein deposits have been strongly linked to the genesis of the neurodegenerative disorder called Alzheimer's disease. The support for the research came from the ERA-NET NEURON (Network of European Funding for Neuroscience Research) project, which backed the MIPROTRAN project involved in the study. ERA-NET NEURON, for its part, received nearly EUR 3 million under the ERA-NET scheme of the Sixth Framework Programme (FP6). The study was recently published in the journal Science. Alzheimer's disease is the most common form of dementia that starts later in life and where the symptoms gradually worsen. It is incurable and scientists are still largely in the dark about what causes the disorder. Most often, it is diagnosed in people over 65 years of age although the less-prevalent early-onset Alzheimer's can occur much earlier. There are over 27 million sufferers worldwide and the disease is predicted to affect 1 in 85 people globally by 2050. In this latest study, which aimed to gain a greater understanding of the disease, scientists at the Hertie Institute of Clinical Brain Research at the University of Tübingen (UT) in Germany and the German Center for Neurodegenerative Diseases (DZNE) injected amyloid-containing brain tissue from older mice into the abdomens of younger mice. Several months after the injections, the younger mice showed evidence of amyloid in their brains. Alzheimer's disease and a brain vascular disorder called cerebral beta-amyloid angiopathy are characterised by the accumulation of a protein fragment known as Abeta. In Alzheimer´s disease, misfolded Abeta is deposited mainly in so-called amyloid plaques, whereas in cerebral beta-amyloid angiopathy, the Abeta protein aggregates in the walls of blood vessels, interfering with their function and, in some cases, causing them to rupture with subsequent intra-cerebral bleeding. In 2006, Tübingen researchers, led by Professor Mathias Jucker, reported that injecting dilute extracts from Alzheimer's disease brain tissue, or from Abeta-laden mouse brain tissue, into the brains of transgenic mice (genetically modified to produce the human form of Abeta) stimulated Abeta aggregation within the mouse brain. In the current study, the researchers found that Abeta deposition can be induced in the transgenic mouse brain by the intraperitoneal administration of mouse brain extract containing misfolded Abeta. They also found that the time needed to induce amyloid deposition in the brain was much longer for peripheral as compared to direct brain administration. But in both cases, the induced amyloid deposition also triggered several neurodegenerative and neuroinflammatory changes commonly observed in the brains of patients with Alzheimer´s disease and cerebral beta-amyloid angiopathy. 'The finding that mechanisms exist allowing for the transport of Abeta aggregates from the periphery to the brain raises the question of whether protein aggregation and propagation, which may also be involved in other neurodegenerative brain diseases, can be induced by agents originating in the periphery,' Professor Jucker commented. He and his colleagues also suggested that amyloid protein may have prion-like qualities. Prions are made primarily of protein and can be transmitted to trigger brain ailments such as Creutzfeldt-Jakob disease. However, they said that 'despite this remarkable observation and the apparent mechanistic similarities between Alzheimer´s and prion diseases, there is no evidence that Alzheimer's disease or cerebral amyloid angiopathy is transmitted between mammals or humans in the same manner as prion diseases'. The present findings provide new clues on pathogenetic mechanisms underlying Alzheimer's disease, they said, adding that further investigation will likely lead to new strategies for prevention and treatment.
Countries
Germany