Understanding the activation of BAT for improved diabetes treatment
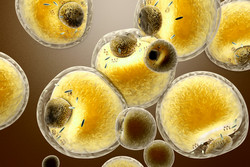
Research into diabetes and obesity has made some huge strides in recent years. And one of the most promising findings is related to the functioning of BAT, home to brown adipocytes. BAT has been revealed to be a major site for lipid breakdown and glucose uptake. In fact, the thermogenic capacity of even small amounts of brown adipocytes has emerged as an attractive target for anti-diabesity (diabetes and obesity) therapies. That’s why, for the past four years, the EU-backed DIABAT (Recruitment and activation of brown adipocytes as preventive and curative therapy for type 2 diabetes) project team has been working to develop innovative, energy-consuming, BAT-centred therapies for at-risk individuals and patients with type 2 diabetes. In order to advance BAT knowledge toward the development of strategies and therapies, DIABAT explored the differentiation, function, dysfunction and physiological regulation of brown adipocytes. The team employed experimental cellular systems and animal models as well as studies on human volunteers using BAT imaging methods for in situ functional analysis. This means that, crucially, the experimental findings are now primed for clinical exploitation. As DIABAT drew to a final close, project manager Dr Tobias Schafmeier from the German Cancer Research Center took some time out to speak about the impressive advances achieved: ‘In the past four years, the DIABAT consortium has made huge progress towards understanding the in vivo activation of BAT by endogenous, nutritional and artificial compounds and has revealed important underlying biological mechanisms. Furthermore, better imaging technology has gained opportunities for functional analysis of BAT in humans and improved BAT-associated diagnostics.’ There is ongoing discussion in the scientific community about the quantitative contribution of BAT to overall energy expenditure in humans. Nevertheless, work performed by DIABAT demonstrated that even in settings where energy expenditure was not significantly increased, the metabolic status of an organism potentially gets substantially improved upon BAT activation. Dr Schafmeier comments, ‘This observation can be explained by the fact that BAT may act as a sink for glucose and lipids thereby ameliorating elevated serum levels of these nutrients in obese conditions. Furthermore, BAT apparently has an endocrine function with an impact on remote tissues as it secretes bioactive substances (BATokines) into the circulation.’ Apart from the main findings on the in vivo activation of BAT, the research team also identified several molecular players that are key in adipocyte differentiation and the conversion of white adipocytes to a brown-like phenotype. ‘Furthermore,’ Dr Schafmeier adds, ‘great progress has been made in developing methodology and techniques for studying adipose tissue. DIABAT research resulted in more than 100 peer reviewed publications and DIABAT researchers released a special issue of Biochimica et Biophysica Acta on brown and white fat.’ The outcomes of the project will certainly primarily be of interest to researchers, as an in-depth understanding of adipocyte differentiation and BAT activation has been gained. However, according to Dr Schafmeier, other professionals dealing with obesity and diabetes are also likely to take an interest in DIABAT’s results: ‘The findings are also relevant for physicians due to improved BAT imaging that has been developed during the project. Additionally, the project results probably will have high impact for nutritionists and manufacturers of dietary supplements, exemplified by the identification of novel nutritional compounds that have the potential to induce white adipose tissue browning.’ Ultimately, says Dr Schafmeier, it will be patients with obesity-associated metabolic dysfunction including type 2 diabetes who stand to gain the most from DIABAT’s four-year efforts: ‘Given the improvements in BAT imaging that have been made by the consortium, subjects could now be more efficiently stratified according to their amount of BAT, and targeted therapies could be pursued at least in BAT-positive individuals. Food supplements that have been characterised in the project have the potential to improve whole-body metabolism by inducing/activating BAT.’ As for the future, Dr Schafmeier is certain that the strong connections that have been established between partners during the project will endure: ‘The consortium partners agreed that they will take measures to preserve the enthusiastic and productive spirit of DIABAT. Regular physical meetings will help to continue the network. Funding for networking activities will be acquired and future funding opportunities either for the consortium-as-a-whole or for smaller subgroups (for example, an application for a Marie-Sklodowska-Curie ETN) will be sought.’ For more information, please visit: DIABAT
Countries
Germany